March is National Brain Injury Awareness Month, an opportunity to pause and remember that traumatic brain injury, or TBI, is one of the leading causes of disability and death in the United States. According to the Centers for Disease Control and Prevention, TBI’s contribute to about 30 percent of all injury deaths. Of equal concern, people who survive serious TBI’s may suffer the effects for as long as they live.
Tragically, most traumatic brain injuries could have been prevented.
“Traumatic brain injury can be a devastating diagnosis because one moment the person is normal, and the next moment, life has changed abruptly,” says Brad Skidmore, MD, a neurosurgeon with Mayfield Brain & Spine. “TBI affects all aspects of our lives. Everyone thinks about the physical impact, but personality and cognition are also affected. Cognitively, an individual can be devastated.”
Head injuries range from mild to moderate to severe, but all should be taken seriously. A concussion in which an individual loses consciousness for a brief time or not at all may qualify as a “mild” TBI. But even mild brain injuries can have serious long-term consequences. They can produce symptoms that include headache, irritability, and inability to concentrate.
If you suspect that you or a loved one has suffered a concussion, seek immediate medical attention, Dr. Skidmore says. “Obviously, if it is a major traumatic brain injury, everyone goes to the hospital. But even if the injury appears minor, it should be checked out. This is why trainers are pulling athletes to the sidelines after a collision or blow to the head.”
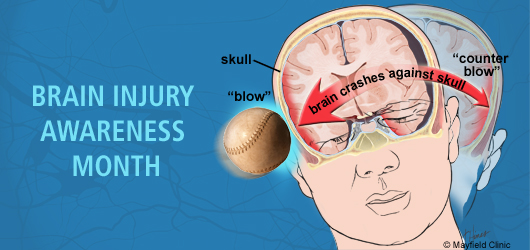
Moderate brain injuries involve a longer period of lost consciousness, while serious injuries can be fatal or life-threatening. Major TBI, often from a fall, vehicular accident, sports accident, or physical attack, involve two stages of trauma. The first involves the initial blow to the head. The second involves the body’s response to the blow, a secondary wave of damage caused by inflammation that causes the brain to swell and press against the skull. Inflammation also spawns spreading depolarizations, or “brain tsunamis,” travelling waves of brain dysfunction that spread out from an injury site and contribute to worse outcomes in patients.
Despite years of research, there is still no proven medical treatment for neurotrauma. As a result, prevention remains the best medicine. Below is a list of basic rules of prevention:
- Always wear a seat belt, and always secure small children into age- and weight-appropriate car seats.
- Identify a designated driver or hire a cab or ride service after drinking alcohol.
- Never drive while under the influence of drugs.
- Do not talk on a cell phone or send or view text messages while driving.
- Always obey highway laws.
- If you experience seizures, do not drive until cleared by your doctor.
- Always wear a helmet when bicycling, skateboarding, or riding a motorcycle or ATV.
- Wear recommended, protective headgear during contact sports.
- Hold onto handrails when using stairs.
- Never stand on the top step of a ladder.
- Wear skid-resistant footwear in wintery weather.
- When swimming, jump feet-first into unfamiliar bodies of water.
- Dive only into water that is at least 10- to 12-feet deep.
To learn more about traumatic brain injury, please visit:
Centers for Disease Control and Prevention >
Brain Injury Association of Ohio >
ThinkFirst National Injury Prevention Foundation >
— Cindy Starr