A new technique from Mayfield spine surgeons, detailed in the September issue of World Neurosurgery, may help prevent complications after fusion surgery to correct adult spinal deformity (ASD). Lead author Dr. Zachary Tempel says findings looked promising in the first series of 20 patients with ASD who underwent this technique to restore spinal alignment. Co-authors included Mayfield surgeons Dr. Bryan Krueger, Dr. Randall Hlubek and Dr. Michael Kachmann.
“One year later, no patient showed failure, either proximal junctional failure (PJF) or proximal junctional kyphosis (PJK),” Tempel writes in the article. “These two complications are most common in the first year after correction surgery, before the bones fuse, and they often interfere with healing. Distributed loading may prevent such complications by ‘softening the landing’ at the junction of fused and non-fused spine.”
Patients with severe ASD who undergo spinal fusion face a risky surgery to correct their deformity. Risks include further neurologic injury or paralysis. But there is also the hope for radical improvement. A patient’s quality of life dramatically improves when spinal alignment can be restored to near normal.

“Distributed loading may prevent such complications by ‘softening the landing’ at the junction of fused and non-fused spine.”
“Patients with ASD can develop debilitating back pain, or be unable to walk or stand upright, or have difficulty breathing or eating,” Dr. Tempel notes. “They can feel isolated and depressed, desperate for a solution.”
These issues are pressing because of global aging of the population. First, more adults have a normal spinal curve that is deforming as a result of injury, age or spinal degeneration. Dr. Tempel cites an estimated prevalence of moderate-to-severe adult scoliosis in 68% of patients older than 60. Medical names for these conditions include scoliosis, kyphosis and scolio-kyphotic deformity.
Second, patients with ASD who undergo this long-segment correction surgery must understand the risks for complications and failure of the construct, says co-author Dr. Krueger.
During corrective surgery for ASD, a long construct of rods and screws is fixed to the patient’s pelvis and then extended to the upper thoracic spine, fixing the spine for fusion and healing. However, these features also create strain at the uppermost junction of the fused and adjacent non-fused spinal segments. With its natural mobility, the non-fused spine absorbs this stress associated with fixation. This junction is where strain occurs, where complications of PJF or PJK develop and where constructs fail.
“The idea behind the distributed loading technique is to reduce this strain and failure at this junction so healing and bony fusion can happen”, says Dr. Tempel, who designed the construct based on biomechanics of the spine and fusion materials. “Selecting rods of varied materials and stiffness, we created a construct customized to each patient’s anatomy and deformity. The titanium or chromium rods, connectors and screws gradually change from rigid at the pelvis to more flexible at its top junction.”
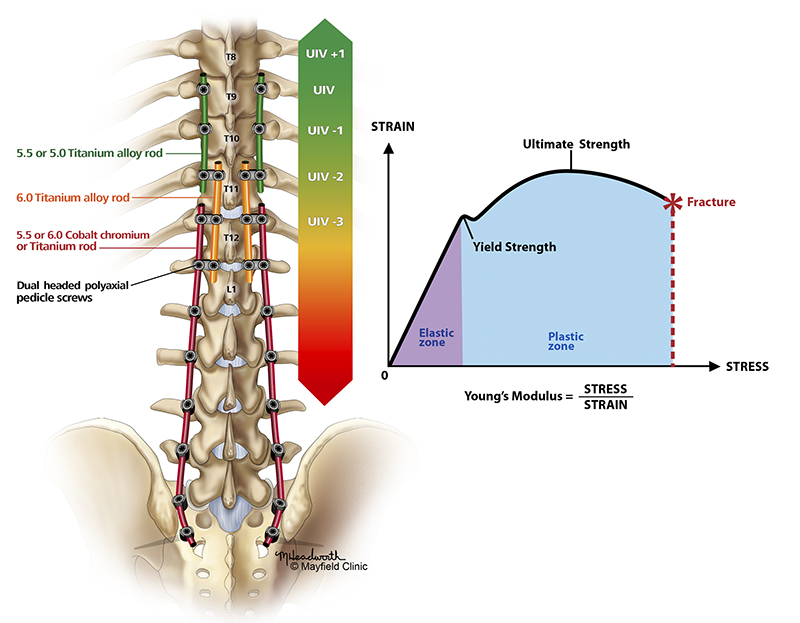
Dr. Krueger adds, “Distributing the load softens the construct’s landing at this junction of fused and normal spine. Thus, it more closely resembles the biomechanics of the normal spine.”
Less strain on the spine brings hope for fewer complications and better healing for patients who will undergo complex spine surgery for ASD.
This study was supported by the Mayfield Education & Research Foundation (MERF) as part of its support for development of surgical innovations. Mayfield has a long history in complex spine surgery and research that included pioneering work by the late Charles Kuntz IV, MD. Authors Tempel, Krueger, Hlubek and Kachmann are part of the MERF research mission to better outcomes for patients with spinal diseases and conditions.
Spine surgeons meet every two weeks at a multi-disciplinary spine conference to discuss complex spine cases and formulate the best strategy of care for each patient. Our patient education program covers spine topics, and the surgical team ensures that patients understand the risks of surgery and have reasonable expectations about the postoperative period of healing. Mayfield physical therapists help patients with various exercise therapies or pain-relieving tools before and after surgery and in planning lifestyle changes to enable a functional recovery.