Mayfield Brain & Spine carries a long history of innovation to serve patients, a spirit that continues today by adapting technology to customize care to each individual case.
Current examples include:
- Patient-specific spinal implants and equipment that recognize even tiny differences in a patients’ anatomy using artificial intelligence and 3D printing capability.
- Operating room systems that marry different imaging and diagnostic programs in one integrated platform, making the operating room more efficient with the potential to improve patient outcomes.
- Adaptive intelligence models that use machine learning and predictive modeling to account for biomechanics of the spine in patient-specific cases to avoid complications after spinal deformity surgery.
Overall, the effect is the same: Mayfield neurosurgeons can improve patient outcomes by harnessing the latest technology and creating individual solutions.
“The path to success in neurosurgery starts well before the patient enters the operating room,” said Dr. Zachary Tempel, part of Mayfield’s Scoliosis and Spinal Deformity team. “We are collaborating with researchers and industry partners so we have hardware and software that allows us to target the disorder with a precision that might have been impossible in previous years.”
Patient-specific spinal implants
Dr. Tempel, for example, works with a manufacturer to create rods used in spine surgery, building the rods to vary in stiffness and flexibility in specific places that match a patient’s unique spine disorder. The individualized approach promotes a biomechanical “soft landing” at the spots where hardware and native spine are joined, according to a whitepaper from Spinal Resources Inc.
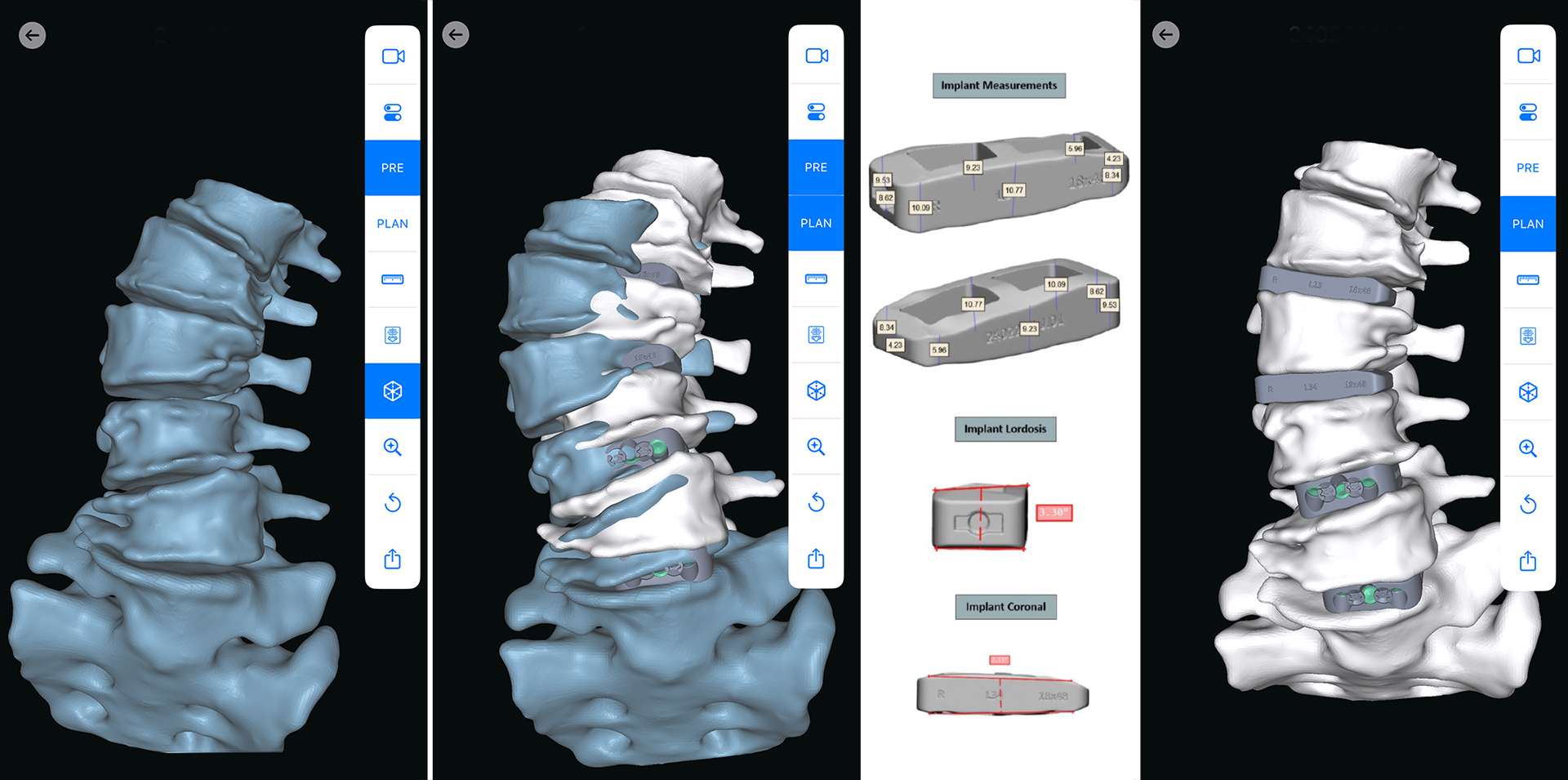
Adaptive intelligence models
Using algorithms that analyze huge data sets can help surgeons shape the spinal procedure, allowing them to predict and avoid post-operative complications. Mayfield neurosurgeon Dr. Bryan Krueger develops a plan, and a biomedical engineering team predicts the outlook for factors including proximal junctional kyphosis, a complication that can develop after surgery, and pelvic tilt. The tool then recommends specifications for a surgical rod and other hardware.
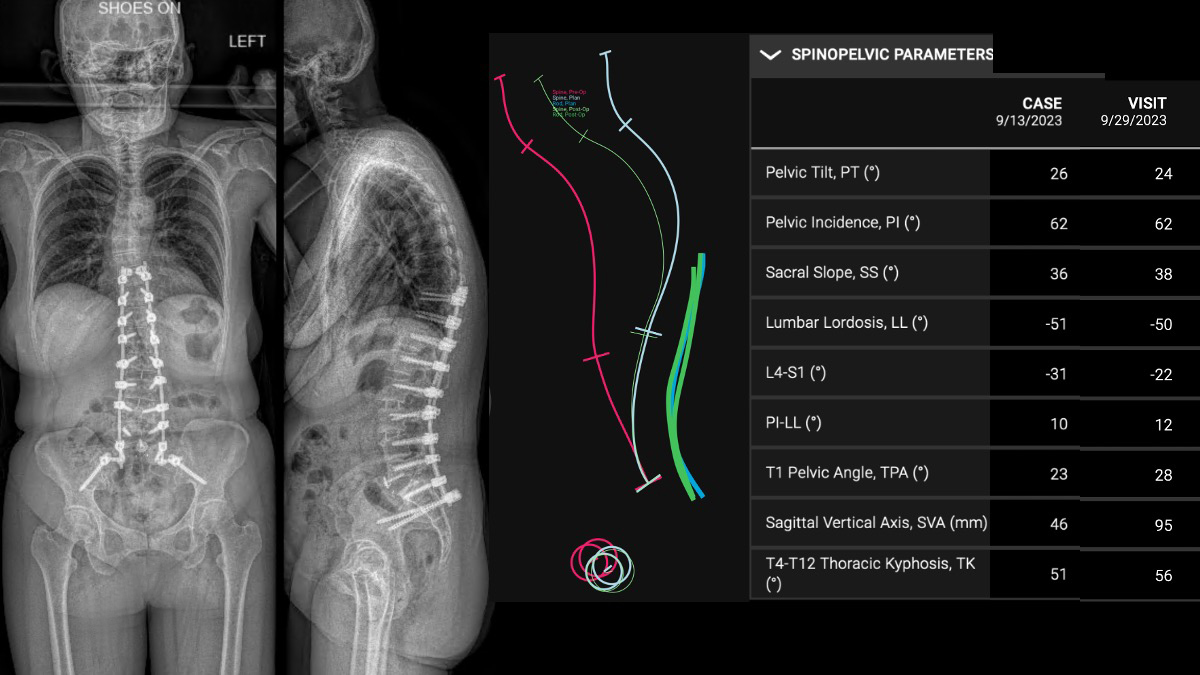
“Once the plan is finalized, they create this patient-specific implant,” Dr. Krueger said of the UNiD Adaptive Spine Intelligence program. He said it provides data analysis and predictive intelligence that can meaningfully improve spine surgery.
“It’s a very personalized experience for the surgeon,” Dr. Krueger said. “AI in surgery can be thought of more as augmented intelligence for the surgeon that enhances the chance for success. We are on the ground floor with this technology, and it’s going to be part of the future.”
Integrated operating room systems
The platforms that guide surgeons as they navigate the narrow corridors in the spine or brain also are a focus of innovation. Mayfield has been a leader by integrating different functions into one unified hardware to improve operating room efficiency. In 2021 at Good Samaritan Hospital, Dr. Michael Kachmann and Dr. Tempel performed the first-ever commercial spinal surgeries in the U.S. using the Pulse® surgical platform.
Dubbed a “smartphone for the operating room,” Pulse integrates multiple functions in one piece of equipment at the surgeon’s fingertips, including radiation reduction, imaging enhancement, rod bending, navigation, intraoperative neuromonitoring and spinal-alignment tools.
That technology continues to advance. Working with collaborators at Miami Valley South Hospital, Dr. Ryan Godinsky recently became the first surgeon in the Dayton area (and one of the first in the country) to use the ExcelsiusHub™ navigation system. The system uses real-time visualization of instrument placement to reduce the reliance on X-ray imaging during spine surgery.

“ExcelsiusHub™ has been a big advancement for our practice and for patients in the Dayton area,” Dr. Godinsky said. “We are able to work faster with navigation because it offers enhanced accuracy as compared to conventional techniques. One of the things I like about it is the alert when accuracy may be compromised. This is a technological enhancement that may result in more efficient operating rooms and surgical solutions for patients.”
After a merger of some of the biggest marketers of these systems, Dr. Kachmann and Dr. Tempel are working closely with TriHealth to bring the latest advances in the Pulse and Excelsius platforms to Good Samaritan and Bethesda North hospitals.
Overall, these technical innovations are designed to help surgeons carry out more precise and effective care plans, Dr. Tempel said.
“When we can shepherd these new technologies to market and validate their safety and efficacy, real people benefit with the latest therapy and improved outcomes,” he said. “This is what Mayfield has been doing for generations – serving patients and changing lives.”