New guidelines for emergency stroke treatment issued yesterday are already benefiting patients at the TriHealth Neuroscience Institute, where Andy Ringer, MD, a neurosurgeon with Mayfield Brain & Spine, is Chief of Neurosciences. The Institute has the specialized imaging and clot-retrieval devices ready and waiting to treat a subset of patients who have small strokes caused by blockages in large arteries.
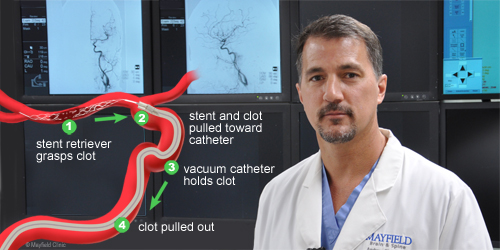
Dr. Ringer took part in two studies published this month that found that patients who had suffered an ischemic stroke many hours earlier did better if their clot was removed with a retrieval device – a procedure called a thrombectomy — than if they were treated with medication alone.
The first clinical trial (DAWN) showed better outcomes up to 24 hours after the stroke began. A second trial (DEFUSE 3), announced yesterday, found that patients who were screened with special imaging up to 16 hours after their stroke did much better after thrombectomy than those treated with medication alone.
The American Heart Association/American Stroke Association announced its new guidelines yesterday at the International Stroke Conference in Los Angeles. The guidelines recommend that “large vessel strokes can safely be treated with mechanical thrombectomy up to 16 hours after a stroke in selected patients. Under certain conditions, based on advanced brain imaging, some patients may have up to 24 hours. The previous time limit was six hours.”
“This is a dramatic change in the way we consider patients as candidates for emergency care,” Dr. Ringer says. “It wasn’t that long ago that we thought that after 3 hours we couldn’t do anything. That went up to 4.5 hours, then up to 6 hours. And now all of a sudden it’s 24 hours. It’s a big change in the way we approach it.”
The widely expanded window of treatment applies to a small subset of stroke patients who wake up with stroke symptoms or for some other reason do not know when their stroke began. They also must have experienced a certain type of stroke that is diagnosed with specialized MRI or perfusion CT scans.
“You have to prove that the territory of the stroke is smaller than a certain threshold, but the artery that is blocked is large,” Dr. Ringer explains. “In other words, not all of the territory of the brain that is normally fed by that artery has been damaged. If that is the case, we assume that there is much more brain tissue in there that is not working right now but is not dead yet. So if we get the clot out, the stroke stays small and the patient can recover.”
Dr. Ringer cautions that having a small stroke after a large vessel has been closed for more than 6 hours is the exception, not the rule. “Many people get screened for these protocols but don’t meet the criteria for treatment because their stroke is too large,” he says. “In that situation there’s a risk we could make things worse, and the chance that we could make things better is very low.”
Dr. Ringer has already treated patients with acute stroke who woke up with stroke symptoms. “We had no idea how long the stroke had been going on, but it was something less than 24 hours,” he says. “We did specialized imaging to show that it was not a large stroke, got the clot out, and the patients made an excellent recovery and went home from the hospital.”
The DEFUSE 3 trial was stopped early because the patients treated with thrombectomy were doing so well.
Dr. Ringer stresses that any stroke is an emergency and should be treated as soon as possible. If you or a loved one experiences the signs or symptoms of stroke, call 9-1-1 immediately.
For information about how to reduce your risk of stroke:
YouTube video In English >
YouTube video In Spanish >
— Cindy Starr