By Robert Whitten, MD
Medicine can be complicated. At times a neurological condition causes double trouble, as when a nerve pinches in two places. It’s what we call a “double crush.”
At Mayfield Brain & Spine, our physicians and staff deal with this and other complex interactions within the nervous system. We use a variety of investigative tools to explore the relationships between our bones, muscles, tendons, ligaments, blood vessels, and nerves, and how they interact to allow us to do the wondrous things the human body and mind can do.
One of our diagnostic tools is the electromyogram (EMG), often used in conjunction with nerve conduction studies (NCS). EMG and NCS are used to study the peripheral nervous system (from the spinal cord to the ends of our hands and feet) rather than the central nervous system (the connections within the brain to the spinal cord). The nerve roots from our neck interweave in our upper chest (brachial plexus) to form trunks that branch out to form the three major nerves (radial, median, and ulnar) to our arms and hands.
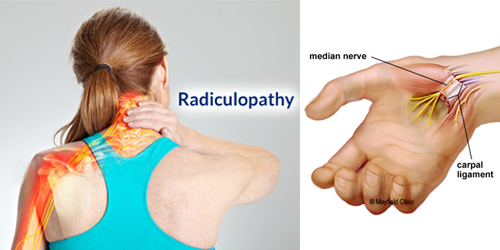
In the upper limb, there are more than 200 ways a nerve can be pinched from the neck to the fingers. Fortunately, many of these are quite rare. One of the more common scenarios involves pinching in the cervical spine where the nerve root leaves the spinal cord, a condition we call cervical radiculopathy. We have 8 cervical nerves (C1 to C8), but those most commonly pinched are C5, C6, and C7.
Carpal tunnel syndrome is the single most common nerve pinch in the arm and actually occurs in the wrist. In about 10% of carpal tunnel cases, there is also a cervical radiculopathy. It is believed that the pinching of the nerve in one area can predispose the remaining nerve to pinching as well. This is the so-called “double crush,” the pinching of the nerve in two distinct locations, in this case the neck and the wrist.
Why does pinching in one area make the nerve more susceptible to a second pinch? Explanations vary from mechanical disruption of axon flow (how nutrients and sustaining compounds travel along the length of the nerve) to immune-mediated attacks on the sensory nerve cell centers (the dorsal root ganglion) or deregulation of the ion channels along the nerve. These channels are integral to the nerve’s ability to carry information to or from the spinal cord.
Additionally, rather than being stationary, our nerves are in constant motion. They glide along the openings in the neck, along the muscles, and around joints when we move our head, neck, shoulders and/or arms. Pinching in one area may compromise this movement, creating increased pressure and tension in other parts of the nerve.
A double crush is also more likely in settings where the overall health of the nerve is compromised. Common underlying problems include diabetes, thyroid disease, excess use of alcohol, immune diseases (like rheumatoid arthritis), peripheral vascular disease, and obesity.
While the double crush most commonly involves carpal tunnel syndrome and C6 (or C8) radiculopathy, it also can involve the ulnar nerve (entrapped at the elbow or less commonly in the hand) and C8 radiculopathy or “handcuff neuropathy” (superficial radial sensory nerve at the wrist) and C5 radiculopathy.
Less frequently it occurs in the leg, which is supplied by 5 lumbar nerve roots (L1 to L5) and two sacral nerve roots (S1 and S2). The most common double crush of the lower limb involves the common peroneal nerve at or near the knee and an L5 radiculopathy. Both can create weakness – a foot drop – which appears farther down the limb.
Dual treatment is important
In double crush syndromes, it is important to recognize both issues, as treating only one area can result in residual symptoms (numbness, tingling, and/or weakness) from the uncorrected second site of impingement. When one of the two entrapments is more predominant on EMG/NCS testing, the surgeon can recommend a two-staged approach that starts by providing relief to the more obvious pinch. If significant residual symptoms remain after the first stage, the second area can then be treated (decompressed) as well.
Sometimes one area can improve with conservative care. In this situation, surgery can be limited to the second area of concern. When both problems require surgery, some patients opt to have them treated in a single operation.
Being aware of the possibility of a double crush, and looking for it when clinically indicated, improves the overall likelihood of successful treatment, whether surgical or conservative.
Robert Whitten, MD, is a physical medicine & rehabilitation specialist with Mayfield Brain & Spine.
References
- https://www.ncbi.nlm.nih.gov/pubmed/3275922 (Orthop Clin North Am. 1988 Jan;19(1):147-55).
- https://www.ncbi.nlm.nih.gov/pubmed/26306807 (J Am Acad Orthop Surg. 2015 Sep;23(9):558-62).
- https://www.ncbi.nlm.nih.gov/pubmed/27751780 (J Hand Surg Am. 2016 Dec;41(12):1171-1175).
- https://n.neurology.org/content/49/1/21 (Neurology. July 01, 1997; 49 (1)).
- https://www.mskscienceandpractice.com/article/S1356-689X(11)00078-6/fulltext
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3192889/