Q: What is adjacent segment disease?
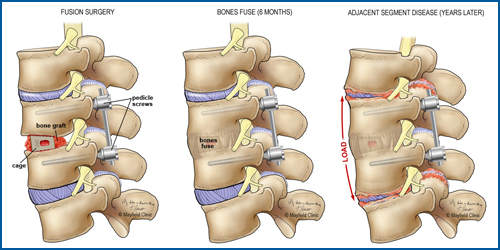
A: Adjacent segment disease (ASD) is a condition that sometimes occurs after a spinal fusion surgery to join or “lock” two or more bones together, stopping the natural motion at that level. Degenerative changes develop on the discs and joints above or below the level where a previous surgery was performed. It is also known as transitional syndrome or adjacent segment degeneration.
Q: How and why does it develop?
A: Adjacent segment disease has two main causes.
- Aging: A natural degenerative process takes place in the spine. As we age, the cushioning discs in our spine dry out and the disc space gradually collapses and loses its normal height. Because the moveable spine works like links in a chain, weakness at one link transfers additional stress and pressure onto the next link. This stress can lead to symptoms when the bones become misaligned, when the nerves become pinched, or when the spine becomes unstable.
- Fusion Surgery: Fusing / locking bones together is thought to potentially accelerate degeneration by increasing the stress and motion above and below the fusion level. However, not everyone with a spine fusion develops ASD and not all spine fusions are the same. Minimally invasive techniques that disrupt fewer muscles and ligaments supporting the spine have the potential to lessen the risk that patients will develop adjacent segment disease. Furthermore, careful attention to optimizing the spinal alignment during the fusion process appears to be critical in minimizing the risk of ASD.
Controversy remains over whether adjacent segment disease is caused by the aging process alone or whether spine operations (fusions) accelerate the process.
Q: Is adjacent segment disease more likely to develop in one area of the spine than in another?
A: Yes. Studies have shown that adjacent segment disease is more likely to develop in the neck (cervical spine) and low back (lumbar spine) than in the thoracic (chest-level) region. This is likely because the cervical and lumbar spine are the most mobile regions of the spine, while the thoracic spine is essentially immobile because of our ribs.
Q: What percentage of fusions lead to this condition?
A: The risk of developing ASD after fusion surgery is variable depending on the initial spine problem, your age and bone health, and the number of levels fused. In general, the risk is 2% to 14% per year in the lumbar spine (Harrop 2008) and 3% per year in the cervical spine (Hilibrand 1999). The re-operation rate 10 years after cervical fusion is 22% (Lee 2015). However, our understanding of adjacent segment disease has evolved, and minimally invasive techniques have been shown to significantly decrease the incidence of this condition. Furthermore, meticulous attention to spinal alignment during the fusion operation reduces the chance that a patient will develop adjacent segment disease. Patients who are fused without the proper amount of lordosis – a forward curvature – in the lumbar or cervical spine have been shown to have worse outcomes.
Q: What can patients do to prevent it?
A: One modifiable risk factor that patients can optimize before and after surgery is weight. Patients who are overweight or obese have a higher risk of complications in general, but also have a higher likelihood of developing adjacent segment disease. This is due to the increased loading of the spine – the amount of weight that the spine is required to support. Additional loading causes increased stress to the adjacent levels and accelerates the degenerative process.
The use of tobacco or vaping products, which contain nicotine, is another risk factor that accelerates the degenerative process throughout the spine and may potentially increase the risk of adjacent segment disease. Patients who smoke or vape should stop prior to surgery to maximize healing and ensure a successful fusion. They should remain nonsmokers indefinitely for the continuing health of their spine and their overall well-being.
Q: How is adjacent segment disease treated?
A: Adjacent segment disease is treated similarly to most spine conditions. Conservative, non-surgical measures such as exercise, physical therapy, and epidural steroid injections are the initial line of treatment. The hope is that patients can avoid a second surgery. If these interventions fail to provide lasting relief and surgery is required, we target the symptomatic level with the most effective and minimally invasive approach available.
Q: Should I consider artificial disc replacement instead of fusion to reduce the risk of ASD?
A: Artificial disc replacement (arthroplasty) has shown promise as an effective surgical option in the cervical spine. The device preserves motion at the fusion level and is thought to protect against adjacent segment disease by causing less stress at the adjacent levels than a fusion. However, not all patients are good candidates for a disc replacement.
Q: What advice do you give your patients after they undergo a fusion?
A: Patients will necessarily go through a healing process after a fusion. I remind patients that we are operating in order to get them back to doing the things they love doing in life. Our goal is to get our patients back to being as active as possible and to re-engaging with life as soon as possible.
Randall Hlubek, MD, is a neurosurgeon and spine specialist with Mayfield Brain & Spine. Learn more about spine conditions at MayfieldClinic.com.